ENT Department Introduction

Otorhinolaryngology abbreviated ORL and also known as otolaryngology, otolaryngology – head and neck surgery (ORL–H&N or OHNS), or ear, nose, and throat (ENT) is a surgical subspeciality within medicine that deals with the surgical and medical management of conditions of the head and neck. Doctors who specialize in this area are called otorhinolaryngologists, otolaryngologists, head and neck surgeons, or ENT surgeons or physicians. Patients seek treatment from an otorhinolaryngologist for diseases of the ear, nose, throat, base of the skull, head, and neck. These commonly include functional diseases that affect the senses and activities of eating, drinking, speaking, breathing, swallowing, and hearing. In addition, ENT surgery encompasses the surgical management of cancers and benign tumors and reconstruction of the head and neck as well as plastic surgery of the face and neck.
What do otolaryngologists treat?
Ear: Otolaryngologists are trained in the medical and surgical treatment of hearing loss, ear infections, balance disorders, ear noise (tinnitus), nerve pain, and facial and cranial nerve disorders. They also manage congenital (birth) disorders of the outer and inner ear.
Nose: Care of the nasal cavity and sinuses is one of the primary skills of otolaryngologists. Otolaryngologists diagnose, manage and treat allergies, sinusitis, smell disorders, polyps, and nasal obstruction due to a deviated septum. They can also correct the appearance of the nose (rhinoplasty surgery).
Colon Polyps-ENT Introduction
Rhinitis Introduction
Rhinitis, also known as coryza,is irritation and inflammation of the mucous membrane inside the nose. Common symptoms are a stuffy nose, runny nose, sneezing, and post-nasal drip.
What is Nonallergic rhinitis?
Nonallergic rhinitis involves sneezing or a stuffy, drippy nose. It can be a long-term problem, and it has no clear cause. The symptoms are like those of hay fever, also called allergic rhinitis. But nonallergic rhinitis isn’t caused by allergies.
Nonallergic rhinitis can affect children and adults. But it’s more common after age 20. Factors that trigger the symptoms vary from person to person. The triggers can include some:
Dust, fumes and other irritants in the air.
Weather changes.
Medicines.
Hot or spicy foods.
Long-term health problems.
Health care providers often first make sure a person’s symptoms aren’t caused by allergies. So you may need skin or blood tests to find out if you have allergic rhinitis.
Symptoms
Nonallergic rhinitis symptoms often come and go year-round. Your symptoms might include:
Stuffy or runny nose.
Sneezing.
Mucus in the throat.
Cough.
Nonallergic rhinitis most often doesn’t cause an itchy nose, eyes or throat. That symptom is linked with allergies such as hay fever.
When to see a doctor
See your health care provider if you:
Have serious symptoms.
Haven’t gotten relief from home remedies or medicines you bought at a store without a prescription.
Have bad side effects from medicines.
Causes
The exact cause of nonallergic rhinitis is unknown.
But experts do know that nonallergic rhinitis happens when blood vessels in the nose expand. These blood vessels fill the tissue that lines the inside of the nose. Many things could cause this. For instance, the nerve endings in the nose might react to triggers too easily.
But any cause brings on the same result: swelling inside the nose, congestion or lots of mucus.
Triggers of nonallergic rhinitis can include:
Irritants in the air. These include dust, smog and cigarette smoke. Strong odors such as perfumes also can cause the symptoms to start. So can chemical fumes, including fumes some workers might get exposed to at their jobs.
Weather. Changes in temperature or humidity can trigger swelling in the lining of the nose. This can cause a runny or stuffy nose.
Infections. Illnesses caused by a virus often cause nonallergic rhinitis. These include a cold or the flu.
Foods and drinks. Nonallergic rhinitis can happen when you eat. Hot or spicy foods are the main triggers. Drinking alcohol also can cause the tissue that lines the inside of the nose to swell. This can lead to a stuffy nose.
Some medicines. These include aspirin and ibuprofen (Advil, Motrin IB, others). High blood pressure medicines such as beta blockers also can cause symptoms.
Medicines that have a calming effect, called sedatives, can trigger nonallergic rhinitis too. So can medicines for depression. Birth control pills and medicines that treat erectile dysfunction also can trigger the symptoms. And using decongestant nose spray or drops too often can cause a type of nonallergic rhinitis called rhinitis medicamentosa.
Hormone changes. These can be due to pregnancy, periods or birth control use. Hormone problems that may trigger nonallergic rhinitis include a condition that happens when the thyroid gland doesn’t make enough thyroid hormone. This is called hypothyroidism.
Issues linked with sleep. Lying on your back while you sleep can trigger nonallergic rhinitis. Acid reflux that happens overnight also can be a trigger.
Risk factors
Things that can make you more likely to get nonallergic rhinitis include:
Breathing in some types of unclean air. Smog, exhaust fumes and tobacco smoke are a few of the things that can raise the risk of nonallergic rhinitis.
Being older than age 20. Most people who get nonallergic rhinitis are 20 or older. That makes it different from allergic rhinitis, which people often have when they’re younger than 20.
Using nose sprays or drops for a long time. Don’t use store-bought decongestant drops or sprays oxymetazoline (Afrin, Dristan, others) for more than a few days. A stuffy nose or other symptoms might get worse when the decongestant wears off. This is often called rebound congestion.
Getting pregnant or having periods. Congestion in the nose often gets worse during these times due to hormone changes.
Being exposed to fumes at work. In some lines of work, fumes from supplies can cause nonallergic rhinitis to start. Some common triggers include construction materials and chemicals. Fumes from compost also can be a trigger.
Some health problems. Some long-term health problems can cause nonallergic rhinitis or make it worse. These include diabetes and a problem that happens when the thyroid gland doesn’t make enough thyroid hormone.
Complications

Nasal polyps
Nasal polyps are soft, noncancerous growths on the lining of the nose or sinuses. They often occur in groups, like grapes on a stem.
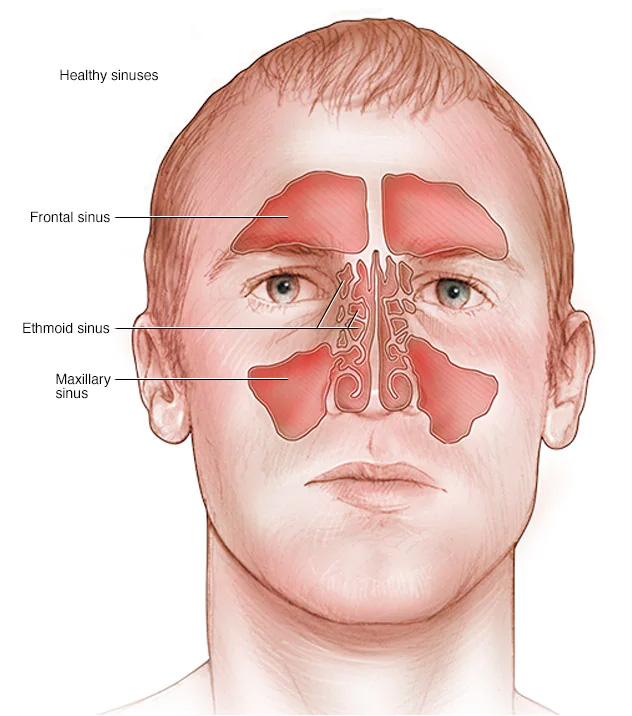
Healthy sinuses
Sinuses are cavities around nasal passages. If the sinuses become inflamed and swollen, a person may develop sinusitis.
Nonallergic rhinitis might be linked to:
Nasal polyps. These are soft growths that form on the tissue that lines the inside of the nose. Polyps also can form on the lining of the spaces inside the nose and head, called sinuses. Polyps are caused by swelling, also known as inflammation. They’re not cancer. Small polyps might not cause problems. But larger ones can block the airflow through the nose. That makes it hard to breathe.
Sinusitis. This is swelling of the sinuses. Long-term congestion in the nose due to nonallergic rhinitis can raise the risk of sinusitis.
Trouble with daily life. Nonallergic rhinitis might affect your work or school grades. You also might need to take time off when your symptoms flare or when you need a checkup.
Prevention
If you have nonallergic rhinitis, take steps to ease your symptoms and prevent flare-ups:
Learn your triggers. Find out what factors cause your symptoms or make them worse. That way you can stay away from them. Your health care provider can help you learn your triggers.
Don’t use decongestant nose sprays or drops for too long. Using these medicines for more than a few days at a time can make your symptoms worse.
Get treatment that works. If you’ve tried a medicine that doesn’t help enough, talk to your health care provider. A change to your treatment plan may be needed to prevent or ease your symptoms.
Throat: Otolaryngologists have expertise in managing diseases of the larynx (voice box) and the upper aero-digestive tract or esophagus, including voice and swallowing disorders.
Head and Neck: In the head and neck area, otolaryngologists are trained to treat infectious diseases, both benign and malignant (cancerous) tumors, facial trauma, and deformities of the face. They perform both cosmetic plastic and reconstructive surgery.
How are otolaryngologist-head and neck surgeons trained?
An otolaryngologist is ready to start practicing after completing up to 15 years of college and post-graduate training. To receive certification from the American Board of Otolaryngology, individuals must first complete college, medical school, and at least five years of specialty training. Next, the physician must pass the American Board of Otolaryngology examination. Some then pursue a one- or two-year fellowship for more training in a subspecialty area. All full-time faculty at Columbia have completed fellowship training in their areas of expertise.
