Prostatitis
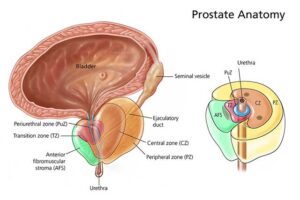 Prostatitis is the inflammation or infection of the prostate gland, which is a small gland located below the bladder and in front of the rectum in males. The prostate gland plays a role in the production of semen. Prostatitis can occur in men of all ages, and it is classified into different types based on its underlying cause and characteristics.
Prostatitis is the inflammation or infection of the prostate gland, which is a small gland located below the bladder and in front of the rectum in males. The prostate gland plays a role in the production of semen. Prostatitis can occur in men of all ages, and it is classified into different types based on its underlying cause and characteristics. Causes
The causes of prostatitis can vary depending on the type of prostatitis. Here are some common causes associated with each type:
1. Acute bacterial prostatitis:
– Bacterial infection: The most common cause of acute bacterial prostatitis is a bacterial infection, often resulting from bacteria entering the prostate gland through the urinary tract. The bacteria responsible for urinary tract infections (UTIs) or sexually transmitted infections (STIs) can reach the prostate and cause infection.
2. Chronic bacterial prostatitis:
– Recurrent infections: Chronic bacterial prostatitis is characterized by repeated or persistent bacterial infections in the prostate gland. The infections can be caused by the same or different bacteria as acute bacterial prostatitis. In some cases, bacteria may form biofilms or hide within the prostate, making treatment challenging.
3. Chronic prostatitis/chronic pelvic pain syndrome (CP/CPPS):
– Non-infectious factors: The exact cause of CP/CPPS is not fully understood, but it is believed to involve various non-infectious factors, such as:
– Inflammation: Chronic inflammation within the prostate gland or surrounding tissues may contribute to the development of CP/CPPS.
– Autoimmune response: Some researchers suggest that an autoimmune response targeting the prostate gland may play a role in CP/CPPS.
– Neuromuscular abnormalities: Dysfunction of the muscles and nerves in the pelvic area, which can cause pain and discomfort, may contribute to CP/CPPS.
– Psychological factors: Emotional stress, anxiety, or previous traumatic experiences may exacerbate symptoms or contribute to the development of CP/CPPS.
4. Asymptomatic inflammatory prostatitis:
– The exact cause of asymptomatic inflammatory prostatitis is not well understood. It is typically diagnosed incidentally during evaluation for other conditions, as there are no noticeable symptoms.
Symptoms
The symptoms of prostatitis can vary depending on the type of prostatitis and the individual. Here are the common symptoms associated with each type:
1. Acute bacterial prostatitis:
– Sudden onset of symptoms: Symptoms may develop rapidly over a few days.
– Fever and chills: You may experience a high fever, accompanied by chills and sweating.
– Pelvic pain: Severe pain or discomfort in the pelvic area, lower abdomen, lower back, or perineal region (between the scrotum and anus).
– Painful urination: Dysuria, which is pain or a burning sensation during urination, is common.
– Frequent urination: You may have an increased urge to urinate frequently.
– Urgency: A feeling of needing to urinate urgently.
– Blood in the urine: Hematuria, or blood in the urine, may occur but is less common.
– Difficulty emptying the bladder: You may experience difficulty fully emptying the bladder, leading to residual urine.
2. Chronic bacterial prostatitis:
– Recurring urinary tract infections: Frequent episodes of urinary tract infections (UTIs) may occur.
– Pelvic pain: Dull, aching pain or discomfort in the pelvic area, lower abdomen, lower back, or perineal region, which may come and go.
– Painful urination: Dysuria, or pain during urination, can be present.
– Frequent urination: Increased frequency of urination.
– Urgency: Feeling a strong and urgent need to urinate.
– Pain or discomfort during ejaculation: Some individuals may experience pain or discomfort during or after ejaculation.
– Sexual dysfunction: Erectile dysfunction (difficulty achieving or maintaining an erection) or reduced sexual desire may occur.
– Blood in the semen: Hematospermia, or blood in the semen, may occasionally be present.
3. Chronic prostatitis/chronic pelvic pain syndrome (CP/CPPS):
– Pelvic pain or discomfort: A persistent or recurring dull ache or pain in the pelvic area, lower abdomen, lower back, or perineal region.
– Painful urination: Dysuria, or pain during urination, may be present.
– Frequent urination: Increased frequency of urination.
– Urgency: A strong and urgent need to urinate.
– Pain or discomfort during ejaculation: Some individuals may experience pain or discomfort during or after ejaculation.
– Sexual dysfunction: Erectile dysfunction, reduced sexual desire, or difficulty achieving orgasm.
– Non-specific urinary symptoms: Some individuals may experience a range of urinary symptoms, such as hesitancy (difficulty starting urination), weak urine flow, or incomplete bladder emptying.
4. Asymptomatic inflammatory prostatitis:
– There are no noticeable symptoms in this type of prostatitis, and it is often diagnosed incidentally during evaluation for other conditions.
Preventions
Prevention strategies for prostatitis depend on the specific type and underlying causes. While some causes of prostatitis may be difficult to prevent, there are measures you can take to reduce the risk of certain types or minimize the severity of symptoms. Here are some preventive measures that may be helpful:
1. Maintain good hygiene:
– Cleanliness: Practice good personal hygiene, including regular washing of the genital area with mild soap and water.
– Avoid irritants: Use gentle, non-irritating personal care products in the genital area, and avoid using harsh soaps, douches, or chemical-laden products that may irritate the urethra and prostate gland.
2. Practice safe sex:
– Use condoms: Consistently and correctly use condoms during sexual activity, which can help reduce the risk of sexually transmitted infections (STIs) that may lead to prostatitis.
– Limit sexual partners: Reducing the number of sexual partners and maintaining monogamous relationships can lower the risk of exposure to STIs.
3. Practice good urinary habits:
– Stay hydrated: Drink plenty of fluids to promote good urinary flow and help flush out bacteria from the urinary tract.
– Urinate regularly: Avoid holding urine for long periods, as it can lead to bacterial growth in the urinary system.
– Empty the bladder completely: Ensure that you fully empty your bladder during each urination to reduce the risk of residual urine and potential bacterial growth.
4. Avoid bladder irritants:
– Limit caffeine and alcohol: Reduce or limit the consumption of caffeine and alcoholic beverages, as they can irritate the bladder and worsen symptoms.
– Stay hydrated: Drinking enough water can help dilute urine and reduce its potential irritant effects on the prostate and urinary tract.
5. Manage stress:
– Stress management: Find healthy ways to manage stress, such as engaging in relaxation techniques, exercise, or activities that help you relax and unwind. High levels of stress may worsen symptoms of prostatitis.
6. Exercise regularly:
– Engage in regular physical activity, as exercise can promote overall health and may help reduce the risk of certain types of prostatitis.
7. Seek prompt treatment for urinary tract infections (UTIs):
– If you experience symptoms of a UTI, such as frequent urination, pain or burning during urination, or cloudy urine, seek medical attention promptly. Early treatment of UTIs can help prevent the spread of infection to the prostate gland and potentially reduce the risk of developing prostatitis.

