Prolaps
Prolapse refers to the displacement or dropping down of an organ or tissue from its normal position. It occurs when the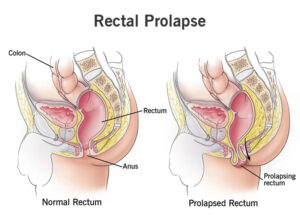 supporting structures that hold the organ or tissue in place weaken or become damaged, leading to the protrusion or descent of the organ. Prolapse can affect various parts of the body, including the pelvic organs, rectum, bladder, uterus, or even the eyelid.
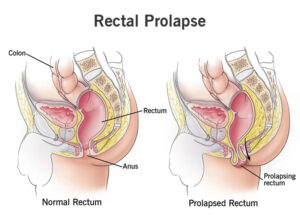
Rectal prolapse involves the protrusion of the rectum through the anus. It occurs when the rectal walls weaken or stretch, allowing the rectum to protrude outside the body. Chronic constipation, straining during bowel movements, weakened pelvic floor muscles, and conditions like chronic diarrhea or cystic fibrosis can contribute to rectal prolapse.
supporting structures that hold the organ or tissue in place weaken or become damaged, leading to the protrusion or descent of the organ. Prolapse can affect various parts of the body, including the pelvic organs, rectum, bladder, uterus, or even the eyelid.
Rectal prolapse involves the protrusion of the rectum through the anus. It occurs when the rectal walls weaken or stretch, allowing the rectum to protrude outside the body. Chronic constipation, straining during bowel movements, weakened pelvic floor muscles, and conditions like chronic diarrhea or cystic fibrosis can contribute to rectal prolapse.
 supporting structures that hold the organ or tissue in place weaken or become damaged, leading to the protrusion or descent of the organ. Prolapse can affect various parts of the body, including the pelvic organs, rectum, bladder, uterus, or even the eyelid.
Rectal prolapse involves the protrusion of the rectum through the anus. It occurs when the rectal walls weaken or stretch, allowing the rectum to protrude outside the body. Chronic constipation, straining during bowel movements, weakened pelvic floor muscles, and conditions like chronic diarrhea or cystic fibrosis can contribute to rectal prolapse.
supporting structures that hold the organ or tissue in place weaken or become damaged, leading to the protrusion or descent of the organ. Prolapse can affect various parts of the body, including the pelvic organs, rectum, bladder, uterus, or even the eyelid.
Rectal prolapse involves the protrusion of the rectum through the anus. It occurs when the rectal walls weaken or stretch, allowing the rectum to protrude outside the body. Chronic constipation, straining during bowel movements, weakened pelvic floor muscles, and conditions like chronic diarrhea or cystic fibrosis can contribute to rectal prolapse. Causes
Anal prolapse, also known as rectal prolapse, occurs when the rectum protrudes or falls through the anus. The exact cause of anal prolapse is not always clear, but there are several factors that can contribute to its development:
1. Weakened Pelvic Floor Muscles: The pelvic floor muscles play a crucial role in supporting the organs in the pelvic region, including the rectum. When these muscles weaken or stretch, it can lead to the descent of the rectum and result in anal prolapse. Chronic straining during bowel movements, childbirth, aging, or previous pelvic surgeries can contribute to pelvic floor muscle weakness.
2. Chronic Constipation: Regular straining and difficulty during bowel movements due to chronic constipation can put significant pressure on the rectum. Over time, this increased pressure can weaken the rectal tissues and lead to prolapse.
3. Chronic Diarrhea: Frequent episodes of diarrhea can also contribute to the development of anal prolapse. The constant irritation and inflammation in the rectal area associated with chronic diarrhea can weaken the rectal muscles and supporting structures.
4. Aging: As people age, the tissues and muscles in the pelvic region can naturally weaken and lose their elasticity. This age-related weakening of the supporting structures can increase the risk of anal prolapse.
5. Previous Surgery or Injury: Any prior surgeries or injuries that have affected the pelvic region or anal area can weaken the supporting structures and increase the likelihood of anal prolapse.
6. Genetic Factors: Some individuals may have an inherited predisposition to developing anal prolapse. Certain connective tissue disorders, such as Ehlers-Danlos syndrome, can weaken the connective tissues and increase the risk of prolapse.
Symptoms
The symptoms of anal prolapse, also known as rectal prolapse, can vary depending on the severity of the prolapse and individual factors. Here are some common symptoms associated with anal prolapse:
1. Protrusion or Bulging: The primary symptom of anal prolapse is the protrusion or bulging of the rectum through the anus. Initially, the prolapse may occur during bowel movements and then retract spontaneously. However, as the condition progresses, the prolapse may become more pronounced and persist outside the body even during rest or minor physical activities.
2. Feeling of Fullness or Pressure: Many individuals with anal prolapse experience a sensation of fullness or pressure in the rectal area. It can feel as if something is constantly pressing or bearing down.
3. Discomfort or Pain: Anal prolapse can cause discomfort or pain, especially when the prolapsed tissue becomes irritated or swollen. The pain can range from mild to severe and may be described as aching, pulling, or a sense of heaviness.
4. Difficulty with Bowel Movements: Anal prolapse can interfere with normal bowel movements. Some individuals may experience difficulty passing stool due to the prolapsed tissue obstructing the rectal opening. This can lead to a feeling of incomplete evacuation, straining during bowel movements, and constipation.
5. Mucus Discharge: Anal prolapse can sometimes cause the release of excessive mucus from the rectum. The mucus can be clear or white in color and may result in a constant moist or damp sensation in the anal area.
6. Anal Bleeding: In some cases, anal prolapse may cause bleeding. This can occur due to irritation or friction of the prolapsed tissue against clothing or during bowel movements. The bleeding is typically bright red and may be seen on toilet paper or in the toilet bowl.
Preventions
While it may not be possible to prevent all cases of anal prolapse, there are measures you can take to reduce the risk or minimize the severity of the condition. Here are some preventive strategies:
1. Maintain Good Bowel Habits: Avoid chronic constipation or straining during bowel movements, as they can contribute to the weakening of rectal tissues and increase the risk of anal prolapse. Ensure you have a diet high in fiber, drink plenty of fluids, and establish regular bowel habits. If needed, consider incorporating fiber supplements or stool softeners under the guidance of a healthcare professional.
2. Practice Proper Lifting Techniques: When lifting heavy objects, it’s important to use proper techniques to avoid putting excessive strain on the pelvic floor muscles and rectal area. Bend your knees, keep your back straight, and lift with your legs rather than straining the rectal muscles.
3. Maintain a Healthy Weight: Excess weight can place additional pressure on the pelvic floor muscles and weaken them over time. Maintain a healthy weight through a balanced diet and regular exercise to help reduce the risk of anal prolapse.
4. Avoid Heavy or Repetitive Straining: Activities that involve heavy or repetitive straining, such as heavy weightlifting or intense, prolonged coughing, can strain the rectal area and increase the risk of prolapse. Be mindful of these activities and take appropriate measures to minimize strain and pressure on the pelvic floor muscles.
5. Practice Pelvic Floor Exercises: Strengthening the pelvic floor muscles can help support the organs in the pelvic area, including the rectum. Regularly performing pelvic floor exercises, also known as Kegel exercises, can help maintain muscle strength and tone. Consult a healthcare professional or pelvic floor therapist to learn the correct technique for performing these exercises.
6. Seek Prompt Treatment for Chronic Cough: If you have a chronic cough, such as from smoking or a respiratory condition, it’s important to seek appropriate medical treatment to manage the cough and minimize the strain it places on the pelvic area.
7. Avoid Prolonged Sitting or Standing: Prolonged periods of sitting or standing can increase pressure on the pelvic floor muscles and rectal area. If your work or lifestyle involves extended periods of sitting or standing, take regular breaks to move around and relieve pressure.

